Kenyon Connects
ICD CODING

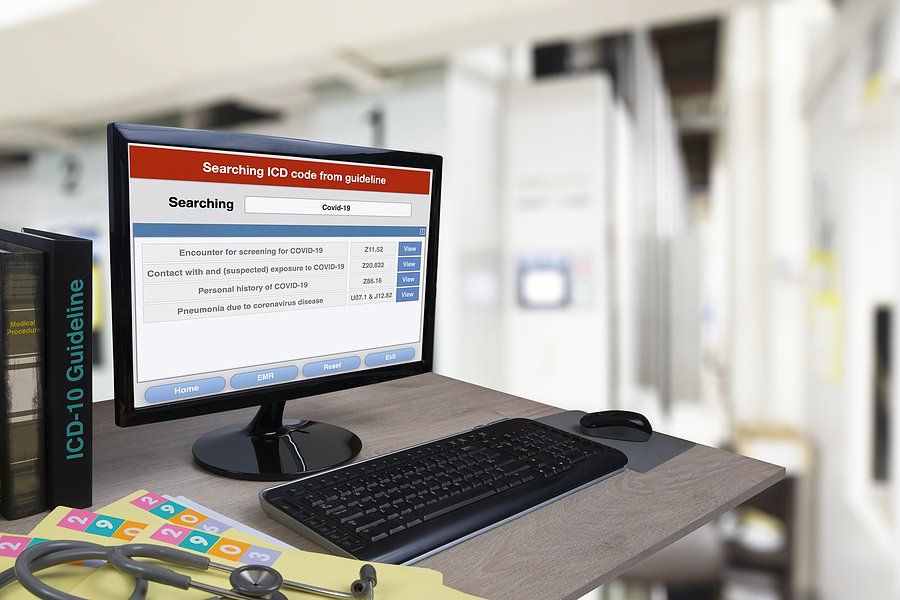
When you think in practical terms, what does your ICD 10 coding mean to the clinicians in your agency? It probably isn't as important as you would like. Realistically, your nursing staff cares about hands on patient care. If you want the code itself to be more meaningful, then you need to attach the concepts of patient care to the ICD coding. You may think the code itself goes hand-in-hand with the care, but this is not always true. As a clinician, there are concepts within the nursing care plan that are automatic and some that are instinctual based upon the body system causing the need for care. It's a given that medication, diet, and disease process teaching are going to be in the care plan (or should be). When you get to disease process, our experience shows the clinician doesn't always run deep into the specifics of the disease when it could lead to valuable interventions being included in care. For example, when clinicians do a care plan related to cardiac disease, are the interventions very broad to include all things related to any type of cardiac disease? If you have a patient with right sided heart failure versus left sided heart failure, how many nurses would assess the patient differently? Would your nurses change the frame of mind to look for distended neck veins or anorexia and nausea if the patient had right sided failure? Would they be in the head space of considering whether the patient's appetite changes are more about just having been in the hospital than about potential venous stasis in the abdomen? The point is that although there are certain interventions that would be the same regardless the type of heart failure, picking up on different symptoms and critically thinking through the cause is often missing in the hustle and bustle of the day-to-day. This is not a judgment on the capabilities of the nurses but more about how our nurses are trained to consider care planning and assessment. We have people for ICD 10 coding now. Most nurses are not in the ICD coding manual looking up their own codes anymore because of the specificity that wasn't the same 25 years ago. So, the nurses go out with an H&P from the hospital or doctors office and develop a care plan. It isn't necessarily with the coding in mind. So, we need to get back to basics when it comes to coding and clinical care. We need to train out staff to look harder at the coding. Our coding departments need to have open communication with clinicians and understand the concepts of care planning to understand if things are missing in the care plans. What about your clinical manager's role? Are these things considered when reviewing care plans? What about your record review process? Are your ICD 10 coders nurses that understand care planning and is it part of the coding process to review the care plan? These are things to consider when you look at your clinical practice as well as your coding solution. At Kenyon Homecare Consulting , we have a comprehensive ICD 10 coding department that can provide education to clinicians, accurate ICD 10 coding, care plan and Oasis review. Call us at 206-721-5091 or contact us online to see if we can help you merge the code with the clinical practice in a way to improve your outcomes and your bottom line. We will offer 5 free recodes to any agency that would like us to check the efficacy of their current coding system or talk about becoming your coding solution.
ICD 10 coding is probably not something consistently on your mind. Normally coding runs like a well-oiled machine unless you find there is a problem. Let’s look at those potential issues and whether or not you are getting the most from your ICD coding dollars. Evaluate Your ICD 10 Coding Solution: The problem with many coding solutions is that they don’t fit the needs of the individual agency. Believe it or not, we still see agencies using ICD 10 coders who are not certified in coding and Oasis. Since the items go hand-in-hand, the people reviewing your charts need to be certified in both. In order to evaluate your current coding solution, you need to ask what the solution actually provides your agency. 1. An ICD 10 Code: If this is all your solution provides, then you need to look at other alternatives. An ICD 10 coding solution should improve your Oasis accuracy, give you useful data in terms of education and documentation, and help increase the dollars you receive for the care you provide. 2. Oasis Review: The individual coding your charts should be reviewing Oasis for accuracy. Your reviewer should identify trends in Oasis errors for the individual clinician and the agency as a whole. This should drive your educational efforts related to Oasis accuracy. In addition, it should also let your agency know if you have clinicians that aren’t making errors in the Oasis tool. If you have an individual nurse or therapist with 95% or greater accuracy on the Oasis, then you can decide if you need to have the tool reviewed by the coder. Look at what the price tag is between having someone code and review the Oasis for accuracy or just code the chart based upon the documentation. Your solution should provide you the data you need to make these decisions. 3. Back-up Plan: Are your coders in-house or outsourced? If in-house, do you have a back-up plan in place should one or more of your coders suddenly be out for an extended period of time? What about your outsourced solution? Many are unaware of the answer to that. If your outsourced provider suddenly loses staff, do they provide a guarantee that your codes won’t be late getting to you? Along the same lines, have you inquired what level of surge your outsourced or in-house solution can provide? The answer is to have a back-up plan in place either way. Even an in-house coding program should have an outsourced provider ready to assist in times of surge or extended absence of your staff. 4. Keeping Up-to-date: How does your solution keep up on coding changes? Ask them. What websites do they search to keep connected? What correspondence is received and what educational offerings do they attend? 5. Compare Your Providers: Look at multiple providers of coding whether you currently have in-house coding or not. Compare and contrast costs versus what is provided by each. Have the outsourced coders recode charts that have already been reviewed. See if the codes match. If they don’t, then find out what one provider sees differently than the other when looking at the same chart. Does one provider’s coding elevate the dollars you receive while still holding true to the rules of coding? The truth is that Kenyon Homecare Consulting has been able to provide agencies up to 20% more in reimbursement than the current coding provider. This is the reason we say for agencies to evaluate the solution they currently use and make sure it continues to consistently meet the needs of your organization. ICD-10 coding is complex and its importance is sometimes overlooked because there are so many other things to do as an administrator. Ultimately, don’t lose dollars or accuracy by going with the wrong coding solution. If you would like Kenyon Homecare Consulting to provide 5 free recodes of charts as a check and balance of your current coding solution or you need us to provide your coding, call us today at 206-721-5091 or contact us online .

Things go quickly in home health. You receive the referral, see the patient, and develop the care plan typically within 48 hours. So, where does ICD 10 coding fit into the mix? Well, it should be an integral cog in your clinical wheel. To keep the process flowing through to billing, ICD 10 coding cannot fall behind. One of the biggest issues we see; Agencies are not prepared for surge. So, how do you make sure you can handle it when things really get busy? In-House ICD 10 Coding: For those of you with in-house coding, do you know what surge your current staff can handle without falling behind? We know that employees can increase productivity to accommodate for a brief period. The question is whether the quality of coding during surge declines. If your staff increases productivity by 20% during a surge time, have you measured the data to determine if HHRG decreases? Are you missing things in the coding because the staff does not have time to dig into the clinical documentation? If so, then what dollars are you missing and what potential coding errors have been made in the process? Outsourced Coding: For those of you that currently outsource, you should know your coding provider’s ability to manage surge. If you come to them tomorrow with an increase in charts that need ICD 10 coding, how many can they handle before they are behind? If you do not know, then you should find out. Using Outsourced Coding as A Surge and Back-Up Plan: Your ICD 10 coding solution does not have to fit into a cookie cutter format. An in-house solution does not mean an outsourced contract is not necessary or beneficial at times. You need to consider surge as well as planned and unplanned absences of current coding staff. If a coder walks into your office and states he or she must be off for the next 3 months for surgery, what will that mean for productivity in that department? What about planned vacations? In the past, you may have just gotten behind and it took some overtime pay to catch up. We do not have that luxury in our timelines anymore. So, put a backup plan in place so you do not miss anything when you are down a coder, or your agency has surging numbers. In the agencies we have worked with, having a backup plan in place helps decrease stress among staff and keep timelines moving in the right direction. Get something in place now before you are in the middle of an issue. Kenyon Homecare Consulting can be your full-time outsourced coding solution or your backup in times of surge or in-house coding absences. We have nurses certified in Oasis and ICD 10 with years of experience in the field. We partner with you to help clinicians improve Oasis accuracy and clinical documentation in the process. Call us today at 206-721-5091 or contact us online to see how we can help you be prepared!

While working with agencies throughout the United States, we have the opportunity to see how many operate. This leads us to talk today about the new Oasis E tool being implemented January 1st 2023. For those who have been in the industry for decades, the implementation of a changed tool is not unusual. In our experience, when agencies educate on Oasis changes, it is normally limited to clinical staff who complete the tool. We need to look at this from the standpoint of ICD 10 coders. It is imperative for your ICD 10 coders to know the assessment tool inside and out. What Are The Changes From Oasis D to Oasis E? CMS updated the Oasis E tool on May 16th, 2022 and provided a PDF to the changes from the February 1, 2022 version. The changes are in line with expansion of Home Health Value Based Purchasing (HHVBP). So, it aligns with outcome based reimbursement. Now more than ever, the Oasis must be marked properly. We see the implementation of 3 different assessments within the tool: Brief Interview for Mental Status (BIMS),Signs and Symptoms of Delirium from the Cognitive Assessment Method (CAM), and the Patient Mood Interview (PHQ 9) which allows for expanded screening for depression. McBee and Associates offers a nice visual crosswalk tool to illustrate the changes from the Oasis D to E. What Does This Do For ICD 10 Coding? It means your Oasis needs to paint the actual clinical picture. Your ICD 10 coding isn't accurate if the documentation doesn't align. This isn't new. Now, HHVBP is going to need to see the outcomes on our patients come to fruition or your reimbursement will suffer. The check and balance of the certified coder means they need to understand the assessment tool as well or better than the nurse who does the assessment. The nurses look at the tool in a different way than the certified ICD 10/ Oasis coder. This is the analogy of the 2 sides of the brain. Putting both of these clinical pieces together is the whole picture and therefore, the whole brain completes the Oasis and coding puzzle. The coder is able to catch discrepancies or address items that don't fully align with the diagnoses based upon other documentation. You may currently have your agency doing coding in-house and if your coders are Oasis and ICD 10 certified, then great. Check their ongoing accuracy and whether it makes financial sense to keep it in-house. Spend the time and money to make sure your ICD 10 coders keep up-to-date on changes. If you don't have certified coders in place, then outsource your coding and Oasis review or you may really be penalized for errors in the tool. If you are looking to outsource, then make sure the person doing the coding is certified in ICD 10 and Oasis. Agencies Can't afford to have Oasis or ICD 10 coding errors cost them money. If you are looking to check the accuracy of your current coding system, outsource your coding, or need someone to provide educational assistance on the new Oasis E tool, Kenyon Homecare Consulting can help. Call us today at 206-721-5091 or contact us online to see how we can help!

In part 1 of our ICD coding series, we looked at an overview as to why smaller agencies can’t afford to do in-house coding. In part 2, we will look at the dollars and cents of coding in-house. If you currently have employees in this role, have you broken down the true cost to your agency and determined productivity standards? Cost And Productivity Of In-House ICD 10 Coding: When we think of productivity in our agencies, we normally talk about clinical employees. Many agencies to not track the number of charts individual coders complete or monitor accuracy in a meaningful way. An RN who is certified in Oasis D and ICD 10 coding should be able to code 12 charts per day or 60 charts per week. If your in-house coders aren’t completing 240 charts a month, you may need to ask why. Our numbers come from a nationwide outsourcing company with many nurse coders on staff. It should also make you ask why you have multiple coders if your admission numbers don’t justify it. It is not uncommon for us to see several in-house coders for agencies with 200 admissions or less. So, let’s do math on cost. The national average according to Zip Recruiter for an RN who is Oasis D and ICD 10 coding certified is $67,571 base salary. If you consider the average overhead rate of 34% of salary ($22,974), then your overall cost per coder is $90,545. Now, this is just the average. So, we realize there are agencies paying less and agencies paying a whole lot more. The same nationwide agency providing productivity numbers stated it is not uncommon for their coders to be paid $78,000 for base salary. Based upon this number, an in-house coder would cost a total of $104,520 ($78,000 base salary + $26,520 overhead). Now, let’s break these costs down for your agency numbers. Based on the national average of $90,545 ($67,571 base salary + $22,974 overhead): 1. An agency averaging 100 admission per month is actually paying $905.45 per chart for a coder of this caliber. 2. 150 admissions per month cost the agency $603.63 per chart for the coder. 3. 200 admissions per month cost the agency $452.72 per chart for the coder. 4. 250 admissions per month cost the agency $362.18 per chart for the coder. 5. 300 admissions per month cost the agency $301.81 per chart for the coder. If we look at these same numbers based on the $78,000 base pay with overhead to total $104,520, the numbers look like this: 1. 100 admissions= $1045.20 per chart for coding 2. 150 admissions= $696.80 per chart for coding 3. 200 admissions= $522.60 per chart for coding 4. 250 admissions= $418.08 per chart for coding 5. 300 admissions= $348.40 per chart for coding Kenyon Homecare Consulting charges $65 for ICD coding and Oasis analysis/ review. Based upon those numbers and the level of expertise and certification, you need to do the math for your agency. If your RN coder is doing 240 admissions per month and is certified and accurate, your in-house coding may work well for you in a cost analysis. In our experience, agencies doing 240 admissions per month with in-house coding normally have several coders on staff. So, the costs for your coding department go up drastically. You may be paying the national average of $90,545 for three or four coders to handle your admissions. Suddenly, you are paying between $271,635- $362,180 per year just to keep your ICD 10 coding in- house. Those same admissions done by Kenyon Homecare Consulting's RN Coding Specialists will save you anywhere from $76,635-$167,180 per year to complete 250 admissions per month. Let Us Be Your Choice For ICD 10 Coding: At Kenyon Homecare Consulting , our ICD 10 coding department works with agencies to help them improve documentation and get the dollars they deserve to service patients. All our coding staff are Oasis and ICD 10 certified RNs who know our industry and the requirements in documentation. Call us today at 206-721-5091 or contact us online to see how we can help you save money and still receive excellent coding accuracy and efficiency.
Over the years, ICD 10 coding has continued to increase in complexity. The days of 3 for diagnosis coding are long gone. Some of us remember those days and how much nicer it seemed. That being said, it is absolutely necessary to have coders who are Oasis and ICD 10 certified. The question then becomes whether or not you keep your coding in-house or whether you should outsource. Reasons To Keep ICD 10 Coding In-House: We don't like change. That's a given, right? We like having coding staff right there alongside everyone else. Access is nice. We like knowing our staff is keeping up-to-date on education and certification. We have peace of mind knowing our staff are trained the way the should be. Often times we have several coders to make sure we don't get behind in times of surge. Here is the biggest issue with all of it: too many agencies can't afford the ICD coding staff they have. Why Can't You Afford It ? Let's face it. profit margins aren't suddenly increasing. For many of you, it is the opposite. Many of you have not considered outsourcing coding. As a part of this series on ICD 10 coding, we will look at when the numbers shows you can fiscally afford to have coders on staff and when you can't. If you are a large regional agency or a national chain, then absolutely. If you do any less than 200 Medicare admissions per calendar month in your agency, then you probably lose money on coding in-house. You need to do a dollars and cents comparison. You need to consider the dollars you put into staff such as insurance benefits , vacation, sick leave, and personal time, etc. When you have long-term staff, these benefit dollars can really add up and cut into your bottom line. Call Kenyon Homecare Consulting: We have a comprehensive coding program that allows you to outsource ICD 10 coding and save you money in the process of providing high-quality coding and Oasis review. We have nurses who complete the coding process while helping your nurses and agency improve Oasis scoring so you don't miss the dollars and outcomes you deserve. Call Kenyon Homecare Consulting today at 206-721-5091 or contact us onlin e to see how we can help you save money. We will complete 5 free recodes to help you check compliance of your current coding solution. We will continue in the next part of this series to break down the dollars of coding in-house versus an outsourced solution, so stay tuned!
In today’s complex world of ICD 10 coding, you need to make sure you receive all the dollars you deserve to care for the patients you see. And although this is something directly related to compliance and reimbursement, we rarely check competency on our ICD 10 coders. Let’s consider what a coding check-and-balance system looks like for your agency. How Do You Do An ICD 10 Check-and Balance? In our industry, we have competencies and supervision on everything and everyone. So, why don’t we check the accuracy of our own coding departments? If you haven’t put a check-and-balance in place, then now is the time. You need to start with a sample of previously coded charts in your agency. We would suggest 5-15 charts depending on the size of your organization and the number of certified coders you have on staff. Contact an outsourced company and ask them to evaluate the charts and code them accordingly. Then evaluate your results. You should see only slight differences. For example: Your agency has 4 diagnoses on the 485. The outsourced company agrees with the diagnoses, but the order in which they are on the 485 if different. If this does not impact the dollars paid to your agency, then it is not a big difference. However, it could mean something different if the second diagnosis is weighted. If the diagnoses are very different, you have a problem. This is a process that should be completed yearly. So, What Comes Next: If you have a problem, then you need to decide what the issue is. Is it a lack of knowledge? Maybe your coding department isn’t requiring the amount of documentation to justify the codes being used. Maybe you still have someone who isn’t coding certified doing Oasis and coding review? Ultimately, Kenyon Homecare Consulting has a comprehensive ICD 10 coding department and can help be your complete solution, your back-up plan, or your ongoing check-and-balance. We will offer your first 5 recodes for free on your check and balance. Call us today at 206-721-5091 or contact us online .

The decision on your ICD 10 coding solution is a big one. If you have in-house coding, then you may not think about outsourcing. It may not have crossed your mind. We don't often think about coding as a part of an agency's strategic plan, but it should be. Ultimately, there are positives and negatives to in-house or outsourcing, but you need to evaluate both to make the best decision for your agency. So, let's give you some ideas on grading your agency's ICD 10 report card. Do You Know If Your ICD 10 Coding Does You Justice? There are so many things to worry about as agency owners and administrators. Coding if often something that is done in the background that often isn't evaluated. The reality is that most agencies do not know if their ICD 10 coding solution is a help or a hindrance. In order to adequately evaluate your program, here are some of the bullet items to consider: 1. Certification: This is not optional. Your ICD 10 coders must be Oasis and ICD 10 certified. It is necessary for compliance to coding rules and to make sure you receive proper reimbursement. 2. Competency: Our industry has a competency requirement for everything, but not coding. Regardless of whether you are outsourced or in-house, you need a check-and-balance system in place. Have a yearly random sample sent to another coding provider and have them recode the charts to see if the results are the same. 3. Job Roles: Does your coder have a dual role? Ultimately, employees who hold multiple positions migrate to the job role they like the most. You can’t afford for coding to take a back seat. 4. Cost: Have you compared the cost of having an ICD 10 coding department in-house versus the cost to have it outsourced? When it comes to cost, you need to look at the all-in cost and not just direct wage. 5. Data: If you are outsourced here, then look at what data you get from your provider. Is your provider tracking Oasis accuracy? Is there an educational component available to clinical staff to help improve Oasis accuracy? Utilize the expertise of your coding provider to make staff better. 6. Reimbursement: How do you compare to others in your state and nationally? Is your HHRG very low? Then you need to evaluate if it is an ICD 10 coding issue, documentation/ Oasis issue, or whether you are not receiving referrals that provide decent reimbursement. It may mean a pivot in your marketing strategy. 8. Turnover Time: How long does it take for your agency to get ICD 10 coding completed from your in-house or current outsourced provider? 9. Back-Up Planning: This is crucial. Most agencies, unless they have a large coding department, are not prepared for decent surge or loss of staff. So, make sure you have an outsourced company to cover you. You may have long term coding staff with lots of vacation and personal time accumulated. You have to make sure it doesn’t hurt you. Let Us Help! At Kenyon Homecare Consultin g, we have a comprehensive ICD 10 coding solution that fits your agency’s needs. Whether you need just coding, coding and Oasis, or a back-up plan, we can help. Call us today at 206-721-5091 or contact us online . We will offer 5 free recodes today to see if your current solution is on the right track!

Distracted By Changes? Keep Your Eye On ICD 10 Coding And You Won't Miss Out On Dollars You Deserve.
When we are asked to look at agencies dealing with financial concerns, we consistently see ICD 10 coding issues contributing to it. Look, things keep getting thrown at us as an industry and that is not going to stop. Therefore, we can't minimize the power of proper coding. Let's look at some of the things that we see in agencies. 5 Common ICD 10 Coding Mistakes: So, agencies often look at cutting costs by way of staffing before they consider coding as a potential issue. So, before you make drastic changes, consider these 5 things: Don't Let Coding Take A Back Seat: As we are still dealing with the effects of the pandemic, we have other things that take up our time and minds. Right now, we are dealing with more regulation changes, expansion of Value-Based Purchasing, EVV, staffing issues, Review Choice Demonstration, and increased costs to provide services. It is not surprising that we are distracted from the importance of ICD 10 accuracy. Here's the thing; it can't take a back seat. Poor coding costs you money and puts you potentially at risk. Coders Aren't Certified In Coding AND Oasis: The 2 quite simply must go together in order to provide accurate coding. ICD 10 Coding goes hand-in-hand with Oasis. Having certification in one without the other doesn't give you the best result. Coders Serve Multiple Roles: Many agencies have coders who also serve as office assistants or other roles within the office. In these cases, we find coding is not done with accuracy and tends to take a back seat to other tasks. Therefore, this individual often doesn't keep up with coding changes as the occur. Again this costs you money. Agencies Don't Consider Outsourcing: When agencies have non-certified coders, it is because they don't want to invest the money or think they don't need it because the Medicare patient load is small. This is a mistake. Our personal experience shows that without certified skilled coding, you lose $500-$1000- per episode. Agencies need to consider outsourcing to make sure they get the dollars they deserve. Outsourcing is a cost-effective way to get quality coding especially when your agency cannot afford someone full time for the job. There Is No Back-Up For Coding: We see agencies don't often have a back-up in place for their current ICD 10 coders. This results in agencies winging it until the coder is replaced or returns from an extended absence. Again, you can't afford to drop back 10 and punt at these times. You need to have a plan in place so you don't lose revenue or time in getting 485's out for signature. Having a back-up plan is good business anyways! Ultimately, in spite of everything going on, you can't be distracted from the importance of proper Oasis scoring and ICD 10 Coding. At Kenyon Homecare Consulting , we provide both services. We can be your coding and oasis outsource solution or your back-up plan during vacations or absences. Our agency will complete 5 free recode of current ICD 10 charts to see if you are on the right coding track! Call us today at 206-721-5091 or contact us online today!
After years of being in the business of homecare consulting, we have seen importance of accurate ICD 10 coding increase. However, those who primarily focus on Medicaid services in their area tend to dismiss the importance of the ICD 10 code. We consistently see these agencies doing coding internally by non-certified coders. Sometimes it's nurses who did the admission or better yet, another staff member such as an office manager who does the codes when needed. Let's talk about why this hurts your from a compliance level and big time when it comes to your financials. But We Only Do A Small Amount Of Medicare: Here's the thing: The method of your ICD 10 coding should not be determined by the size of your Medicare footprint. That's right. Whether you do in-house or outsourced ICD 10 coding is a matter of clinical accuracy, compliance and proper reimbursement. Let's look at each one of those items and why have the proper ICD 10 code is so important. Proper Reimbursement: In our experience, most small Medicare agencies complete in-house coding and it is done by someone with more than one role in the organization. The reality is that when people function in multiple roles within your organization, the individual gravitates to the role he or she most enjoys. In cases where your coder does multiple roles, how many will say coding is what they enjoy the most? Therefore, ICD 10 coding is normally a small task with not much time spent on accuracy. When we see non-certified coders completing this task, it is not uncommon for us to see errors from as small as $100 per episode up to $1,000 per episode missed in potential reimbursement. If you only do 2 Medicare admission per month, then you have lost up to $24,000 of reimbursement with poor coding. While it is understood that small Medicare agencies may not want to invest in the cost of an in-house employee for a small number of codes, it makes sense to outsource the task and get it right. Clinical Accuracy: Whoever completes your coding needs to understand the documentation provided both by the nurses within the assessments but also from outside sources. The individual must understand the Oasis tool and how it fits together to determine the complexity of the patient. The coder must understand what specificities must be present in the coding not only for reimbursement purposes, but also to help guide the care plan. Compliance: This one encompasses everything. You have to make sure the person in charge of your coding isn't doing it improperly. The industry has dealt with case mix creep over the years because CMS thinks this is what happens. If your coder is going to use a specific code, then there must be evidence in the chart to support use of the diagnosis that has more reimbursement attached. We have been asked to evaluate operations in struggling agencies and have seen this happen. The non-certified coder picks the code that will provide the agency more reimbursement without the documentation to back it up. Your agency get set up for takebacks, ADRs, and potential non-scheduled surveys. We also see agencies where the coder tends to stick with the same few codes and you miss out on a ton of reimbursement routinely because the time and attention is not put into coding. Ultimately, ICD 10 coding is so important and not to be dismissed regardless the size of your Medicare footprint. What do you potentially lose both on the clinical and financial side with bad coding? If you have a small Medicare footprint, just make the call and outsource your Medicare coding. It isn't worth the loss of money or risk of non-compliance. If you aren't sure about your agency's coding grade card, call Kenyon Homecare Consulting at 206-721-5091 or contact us online . We will complete 5 free recodes to see if your ICD 10 coding is on point or if it misses the mark!
